Suboxone is most comparable to other medication-assisted treatments such as buprenorphine-only formulations and methadone, all of which help stabilize neurochemical imbalances associated with opioid dependence. Unlike methadone, Suboxone’s combination of buprenorphine and naloxone reduces misuse potential while providing withdrawal and craving control. At Advanced Spine & Rehab in Mesa, AZ 85206, our complete staff of medical professionals is trained in the latest techniques to ensure patients receive safe, evidence-based guidance within a comprehensive, whole-body approach to care.
What Is the 3-Day Rule for Suboxone?
The 3-Day Rule allows clinicians who are not certified to prescribe buprenorphine to administer—but not prescribe—Suboxone for up to 72 hours while arranging ongoing addiction treatment. It permits one day’s medication at a time to manage acute opioid withdrawal and reduce medical risk until appropriate follow-up care is secured. This rule is designed to bridge gaps in access, stabilize patients safely, and prevent deterioration during the critical early stages of opioid withdrawal management.
Is Suboxone Used for a Pain Killer?
Suboxone is not typically used as a primary pain-relief medication. Its buprenorphine component does have analgesic properties, but the medication is primarily designed for treating opioid use disorder by reducing withdrawal symptoms and stabilizing neurochemical pathways. In certain clinically specific cases, buprenorphine-based therapies may be used for chronic pain when other options are ineffective or unsafe. These decisions require careful assessment to ensure proper dosing, monitoring, and avoidance of opioid-related complications.
Does Suboxone Test Positive for Opiates?
Suboxone does not usually test positive for standard opiate panels, which mainly detect substances like morphine, codeine, or heroin. However, specialized drug screens can identify buprenorphine, the active ingredient in Suboxone, as a separate category. Naloxone in Suboxone is not detected on routine tests. Whether buprenorphine appears depends on the type of test ordered, making it important for patients to disclose all medications to ensure accurate interpretation of laboratory results.
What Is the Point of Taking Suboxone?
Suboxone is taken to stabilize individuals with opioid use disorder by reducing withdrawal symptoms, diminishing cravings, and lowering the risk of relapse. Its buprenorphine component partially activates opioid receptors, providing controlled relief without producing the intense euphoria associated with full opioids, while naloxone discourages misuse. This medication supports safer, more predictable neurochemical regulation, allowing patients to regain function, participate in therapy, and progress toward long-term recovery within a structured treatment plan.
How Addictive Is Suboxone?
Suboxone carries a much lower addiction risk than full opioid medications because buprenorphine only partially activates opioid receptors and has a “ceiling effect,” limiting euphoria and respiratory depression. While physical dependence can occur with long-term use, it is clinically different from addiction, which involves compulsive, harmful behaviors. When used as prescribed, Suboxone is considered a safe, evidence-based treatment that helps stabilize brain chemistry, reduce cravings, and support long-term recovery from opioid use disorder.
Common Symptoms That May Prompt Seeking Professional Help and Considering Suboxone Treatment
Escalating Opioid Cravings
Intense, persistent cravings for opioids often signal physiologic dependence and disrupted reward pathways. These cravings can interfere with daily activities, impair decision-making, and increase the risk of unsafe use. When cravings persist despite attempts to cut back, medical evaluation is crucial. Suboxone can stabilize receptor activity, reduce cravings, and support safer recovery. Early intervention helps prevent cycles of misuse, withdrawal, and relapse, improving long-term outcomes and overall functioning.
Withdrawal Symptoms Between Doses
Experiencing withdrawal—such as sweating, shaking, gastrointestinal upset, muscle aches, anxiety, or restlessness—between opioid doses indicates the body has developed dependence. These symptoms often drive continued use to avoid discomfort, reinforcing harmful patterns. Suboxone can ease withdrawal by providing controlled, partial receptor activation. Seeking professional assessment ensures correct diagnosis, safe induction onto medication-assisted treatment, and monitoring to avoid complications associated with unmanaged withdrawal.
Loss of Control Over Opioid Use
Difficulty limiting opioid use—taking more than intended, using more frequently, or spending excessive time obtaining opioids—signals impaired control, a hallmark of opioid use disorder. This pattern increases medical risks, including overdose and injury. Suboxone can provide neurochemical stabilization that reduces compulsive use. Consulting a professional allows for proper evaluation, individualized treatment planning, and integration of behavioral therapies needed for sustained recovery.
Decline in Daily Functioning
Opioid use that disrupts work performance, relationships, sleep patterns, mood stability, or personal responsibilities is a common indicator of a developing disorder. People may notice increased isolation, missed obligations, or decreased motivation. Suboxone therapy can help restore clarity, improve stability, and allow individuals to engage in counseling and support programs. Professional guidance ensures treatment addresses both physical dependence and the broader impact on daily life.
Using Opioids Despite Negative Consequences
Continuing opioid use despite health issues, financial strain, legal trouble, or relationship conflict reflects an escalating disorder. This pattern suggests that neurochemical dependence is overriding self-preservation instincts. Suboxone can reduce this cycle by diminishing cravings and stabilizing brain function. A medical professional can assess risks, provide structured support, and tailor a safe treatment plan to stop progression toward more severe complications.
Medical Causes of the Symptoms When Considering Suboxone Treatment
Opioid Use Disorder (OUD)
OUD alters neurochemical reward pathways, causing persistent cravings, impaired control, and withdrawal symptoms. As dependence deepens, individuals experience functional decline and continued use despite negative outcomes. This condition is the most common medical driver of the symptoms described.
Chronic Pain Conditions
Long-term pain from conditions such as spinal disorders, arthritis, or nerve injuries can lead to prolonged opioid use. Over time, tolerance and dependence may develop, contributing to withdrawal, escalating cravings, and loss of control when pain and medication needs no longer align.
Co-Occurring Mental Health Disorders
Anxiety, depression, PTSD, and other mood disorders can intensify opioid misuse. Individuals may self-medicate emotional distress, leading to dependence, functional decline, and compulsive patterns of use that mirror the symptoms prompting Suboxone evaluation.
Post-Surgical or Injury-Related Opioid Exposure
Short-term opioid prescriptions for acute injuries or surgery can evolve into dependence when pain persists or medication tapering is difficult. Patients may experience withdrawal between doses, rising cravings, and difficulty controlling use as physical dependence forms.
Neurobiological Vulnerability or Genetic Predisposition
Some individuals have genetic or neurochemical differences that increase susceptibility to dependence. These vulnerabilities can accelerate progression from therapeutic use to misuse, triggering cravings, loss of control, and continued use despite consequences.
Medical Treatments and Their Symptom Relief
Suboxone (Buprenorphine/Naloxone)
Stabilizes opioid receptors, reduces cravings, and prevents withdrawal. Helps patients regain daily functioning, decrease compulsive use, and avoid relapse. Often used as a first-line medication-assisted treatment.
Methadone Maintenance Therapy
A full opioid agonist that controls withdrawal and cravings under strict supervision. Reduces relapse risk and supports long-term stabilization for individuals with more severe dependence.
Naltrexone (Oral or Injectable)
An opioid receptor blocker that prevents opioids from producing euphoric effects. Useful after detox to reduce relapse risk in motivated, abstinent patients.
Behavioral Therapy and Counseling
Addresses psychological drivers of opioid misuse, improves coping skills, and reduces emotional triggers. Supports long-term recovery when combined with medication-based treatment.
Medically Supervised Detoxification
Monitored withdrawal management to safely reduce acute symptoms like nausea, anxiety, and restlessness. Prepares individuals for ongoing treatment such as Suboxone or therapy.
Summary
This overview explains common symptoms of opioid dependence, their underlying medical causes, and the top evidence-based treatments that support recovery. It highlights effective solutions such as Suboxone therapy, methadone, naltrexone, supervised detoxification, and behavioral counseling. Each treatment helps reduce cravings, stabilize withdrawal, and restore daily function. By focusing on opioid recovery options, addiction treatment methods, and medication-assisted therapy, this summary provides clear, SEO-optimized guidance for individuals seeking reliable fixes and medical support for opioid-related challenges.
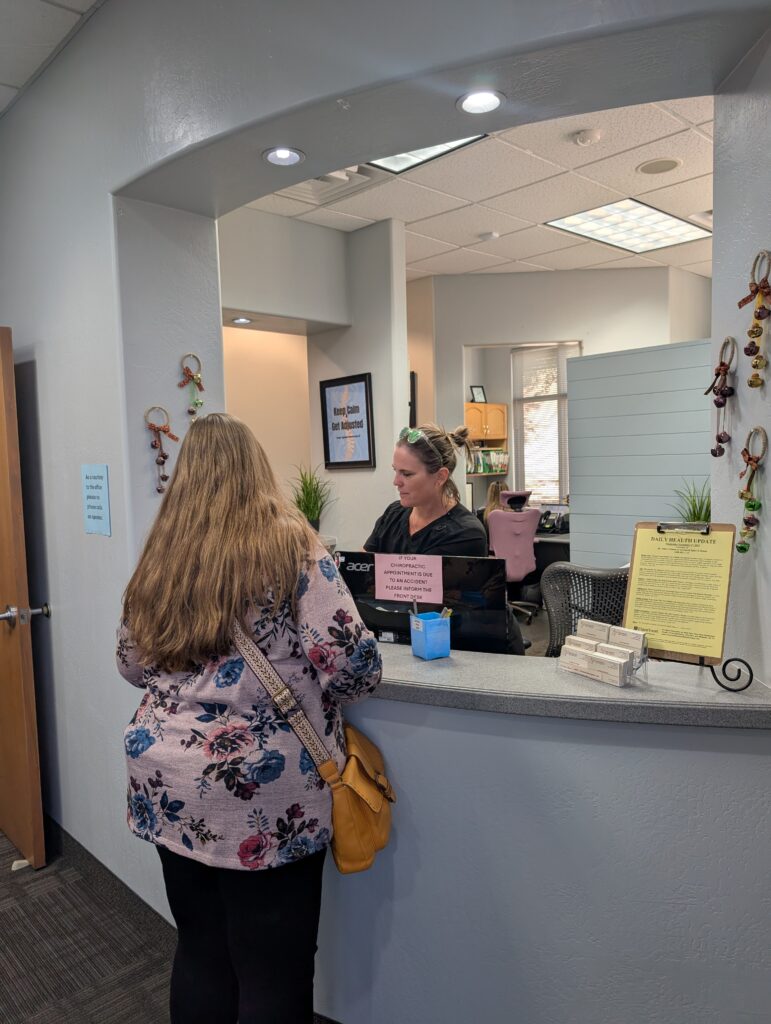
Meet the Professional Staff
At Advanced Spine & Rehab in the Phoenix East Valley, patients are welcomed into a calm, supportive, and encouraging environment designed to promote healing and confidence. Our professional staff is committed to providing individualized care with compassion, understanding, and integrity. Whether you’re beginning your road to recovery or seeking solutions for pain and wellness, our dedicated team takes the time to listen, guide, and design treatment plans tailored to your unique needs. Your comfort, progress, and long-term wellbeing remain our highest priorities.