Trigger point therapy is an evidence-informed manual treatment designed to deactivate hyperirritable muscle knots that contribute to localized and referred pain. By applying precise, sustained pressure, it can reduce muscle tension, improve circulation, and restore normal neuromuscular function. Clinical outcomes often include decreased pain, improved range of motion, and enhanced recovery when combined with corrective care. At Advanced Spine & Rehab in Mesa AZ 85206, a complete staff of medical professionals—trained in the latest treatment techniques—integrates trigger point therapy into comprehensive, patient-centered care plans.
How Effective is Trigger Point Therapy?
Trigger point therapy is widely recognized as an effective treatment for muscle-related pain and dysfunction when applied appropriately. It targets taut bands of muscle fibers that disrupt normal movement patterns and contribute to pain, stiffness, and referred symptoms. Clinical evidence supports its ability to reduce pain intensity, improve range of motion, and enhance muscle performance. Effectiveness is greatest when integrated into a comprehensive care plan that addresses posture, biomechanics, and underlying musculoskeletal or neurologic contributors.
What are the Disadvantages of Trigger Point Therapy?
Trigger point therapy may cause temporary discomfort during or after treatment, particularly in areas of significant muscle tension or chronic sensitivity. Some individuals experience post-treatment soreness similar to delayed-onset muscle soreness, which typically resolves within 24–48 hours. It may be less effective for pain driven primarily by nerve compression, joint pathology, or systemic conditions if used alone. Proper assessment and technique are essential to avoid excessive pressure and ensure it complements, rather than replaces, comprehensive musculoskeletal care.
How Long Does it Take for Trigger Point Therapy to Work?
The response to trigger point therapy varies based on the severity, chronicity, and underlying cause of muscle dysfunction. Some patients notice pain relief and improved mobility immediately or within 24–48 hours after treatment, particularly with acute trigger points. Chronic or long-standing conditions often require multiple sessions to achieve sustained results. Consistent care, combined with corrective exercises and lifestyle modifications, supports longer-lasting improvements and helps prevent trigger point recurrence.
What is the Science behind Trigger Point Release?
Trigger point release is based on neuromuscular and circulatory principles involving dysfunctional motor endplates within skeletal muscle. These hyperirritable areas exhibit sustained muscle fiber contraction, reduced local blood flow, and altered pain signaling. Applying controlled pressure helps normalize muscle spindle activity, restore oxygenation, and reduce excessive acetylcholine release at the neuromuscular junction. This process decreases peripheral sensitization and can modulate central pain pathways, leading to improved muscle function, reduced pain, and enhanced movement efficiency.
Common Symptoms That May Prompt Trigger Point Therapy
Persistent Muscle Pain or Tenderness
Persistent muscle pain that feels deep, aching, or localized is a hallmark sign of active trigger points. This discomfort often worsens with prolonged posture, repetitive movement, or stress and does not fully resolve with rest alone. Palpation of the muscle may reproduce familiar pain or sensitivity. Trigger points can maintain a cycle of muscle guarding and reduced circulation, making targeted manual therapy beneficial for restoring normal muscle tone and reducing ongoing discomfort.
Referred Pain Patterns
Referred pain occurs when a trigger point in one muscle produces pain in a different, predictable area of the body. For example, trigger points in the upper trapezius may cause headaches or neck pain, while gluteal trigger points can mimic sciatica. This phenomenon is related to shared neural pathways and altered pain processing. When pain location does not match imaging findings or joint pathology, trigger point therapy can help address the true muscular source.
Reduced Range of Motion or Stiffness
Trigger points can restrict normal muscle length and elasticity, leading to stiffness and limited range of motion in the neck, shoulders, hips, or back. Individuals may notice difficulty turning their head, reaching overhead, or bending comfortably. This limitation often feels mechanical rather than inflammatory. By releasing sustained muscle contraction and improving local circulation, trigger point therapy helps restore flexibility and supports healthier joint movement patterns.
Muscle Weakness or Fatigue
Muscles affected by trigger points may feel weak, easily fatigued, or unable to perform at normal capacity despite adequate effort. This occurs because dysfunctional muscle fibers cannot generate efficient force and may inhibit surrounding muscles. Over time, this imbalance can contribute to poor posture, compensation, and increased injury risk. Addressing trigger points can improve neuromuscular coordination and allow muscles to function more effectively during daily activities.
Tension Headaches or Jaw Discomfort
Trigger points in the neck, shoulders, and jaw muscles are commonly associated with tension-type headaches and temporomandibular discomfort. Symptoms may include pressure-like head pain, facial tightness, or jaw soreness without clear dental causes. These trigger points can sensitize surrounding nerves and perpetuate pain cycles. Targeted trigger point therapy helps reduce muscular tension, normalize nerve input, and alleviate headache frequency and intensity.
Top Medical Causes Contributing to Trigger Point–Related Symptoms
Chronic Postural Strain
Prolonged poor posture from desk work, device use, or driving places sustained stress on specific muscle groups. Over time, this leads to muscle overload, reduced circulation, and neuromuscular imbalance. These conditions promote trigger point development, contributing to persistent pain, stiffness, referred pain patterns, and functional limitations affecting the neck, shoulders, back, and hips.
Repetitive Use or Overuse Injuries
Repetitive motions in occupational, athletic, or daily activities can exceed a muscle’s ability to recover. Microscopic muscle fiber damage accumulates, leading to localized ischemia and abnormal motor unit firing. This environment fosters trigger points, resulting in muscle tenderness, reduced endurance, restricted motion, and pain that may extend beyond the involved tissue.
Acute Trauma or Microtrauma
Motor vehicle accidents, falls, or sudden muscle strain can directly injure muscle fibers and surrounding soft tissues. Even minor but repeated microtrauma can disrupt normal neuromuscular control. The body responds with protective muscle contraction, which may persist and evolve into trigger points, contributing to chronic pain, weakness, and movement dysfunction.
Spinal Joint Dysfunction
Restricted or abnormal motion in spinal joints alters normal nerve signaling and muscle activation patterns. Muscles surrounding dysfunctional segments may become overactive or inhibited, increasing trigger point formation. This can manifest as localized pain, referred symptoms, stiffness, and headaches, even when imaging findings are minimal or inconclusive.
Psychological Stress and Sleep Disturbance
Chronic stress and poor sleep elevate muscle tone through increased sympathetic nervous system activity. This sustained tension reduces muscle recovery and circulation, making trigger points more likely to develop. Over time, patients may experience widespread muscle pain, fatigue, headaches, and heightened pain sensitivity despite the absence of structural injury.
Top Medical Treatments for Trigger Point–Related Symptoms
Trigger Point Therapy
This manual treatment applies sustained pressure to deactivate hyperirritable muscle fibers. It improves local circulation, normalizes neuromuscular signaling, and reduces referred pain, muscle tenderness, stiffness, and restricted range of motion associated with active trigger points.
Chiropractic Adjustments
Spinal and extremity adjustments restore joint mobility and improve nerve communication. Correcting joint dysfunction reduces abnormal muscle activation, helping relieve muscle tightness, headaches, neck and back pain, and movement limitations linked to trigger point development.
Therapeutic Exercise and Stretching
Targeted strengthening and stretching programs correct muscle imbalances and improve flexibility. These exercises support long-term symptom relief by reducing muscle fatigue, improving posture, and preventing recurrence of trigger points and associated pain patterns.
Soft Tissue Modalities
Techniques such as myofascial release, instrument-assisted therapy, and massage address tissue adhesions and fascial restrictions. These treatments decrease muscle tension, enhance blood flow, and alleviate soreness, stiffness, and referred pain symptoms.
Lifestyle and Ergonomic Modifications
Addressing posture, workstation setup, sleep habits, and stress management reduces ongoing muscular strain. These changes support tissue healing and help minimize chronic muscle pain, tension headaches, and recurrent trigger point activation.
Summary
Trigger point–related pain often develops from postural strain, overuse, trauma, or spinal dysfunction and can lead to muscle tenderness, stiffness, headaches, and reduced mobility. Effective treatment focuses on correcting both symptoms and underlying causes through trigger point therapy, chiropractic adjustments, therapeutic exercise, soft tissue modalities, and ergonomic modifications. These evidence-based approaches work together to restore neuromuscular balance, improve circulation, enhance range of motion, and support long-term musculoskeletal health and injury prevention.
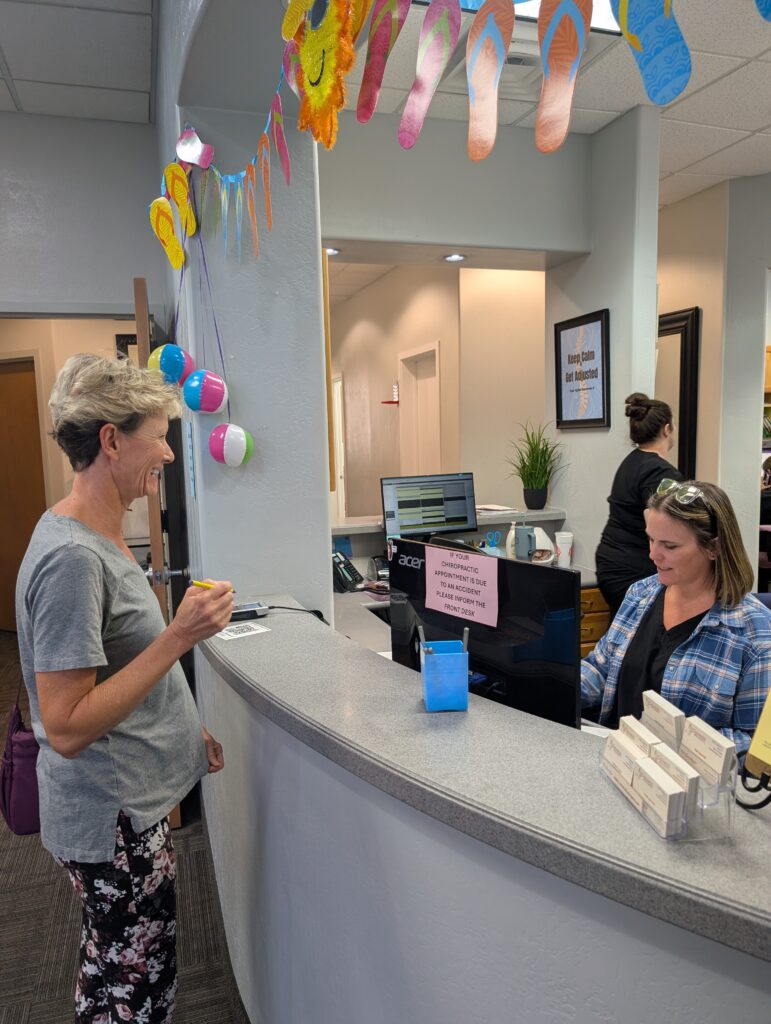
Meet the Professional Staff
At Advanced Spine & Rehab in the Phoenix East Valley, patients are welcomed into a calm, supportive environment focused on individualized care and lasting results. Our professional team is committed to providing treatment with compassion, understanding, and integrity, taking the time to listen and develop care plans tailored to each person’s needs. We guide patients through their recovery with clarity and encouragement, helping them find effective solutions for pain relief, improved function, and long-term wellness.